The Star Player On Your Team.
Following seroconversion, immumoglobulin A (IgA) istoype is the most frequently created antibody in the immune system. This is principally because it dominates the upper respiratory tract, which is usually the first point of contact between pathogen and human. Therefore, it is needed more frequently than the other isotypes. As well as being the most frequent, it is also the second most common in the body, after immunoglobulin G (IgG).
IgA matures into two subclasses; IgA1 and IgA2. IgA1 is a monomer and exists in serum. IgA2 is a dimer and exists in mucus, which is why it is generally known as secretory IgA. Secretory IgA can provide protective or sterilising immunity to a pathogen, unlike IgG.
SARS-CoV-2 is a respiratory virus. It first comes into contact with the immune system in the upper respiratory tract. It is ‘armed’ through S1 subunit cleavage in the upper respiratory tract; it binds to apical ciliated epithelial cells in the upper respiratory tract; cellular fusion & entry is in the upper respiratory tract; the replication process occurs in the upper respiratory tract and replicated new virions are released in the upper respiratory tract for expulsion through mucal excreta. The accumulation of virions and/or viral infection – viral load – occurs in the upper respiratory tract. You can see that there is a pattern here. If you want to an effective viral countermeasure, target the upper respiratory tract which means focusing upon IgA.
We have been vehement critics of the obsession with IgG as the target antibody stimulated by vaccine or antiviral candidate. The structural spike protein is the obvious but wrong choice for developing treatments, principally because of antigen shift. This dynamic glycan shielding is SARS-CoV-2’s natural defence; its adaptive camouflage to aid immunoevasion.
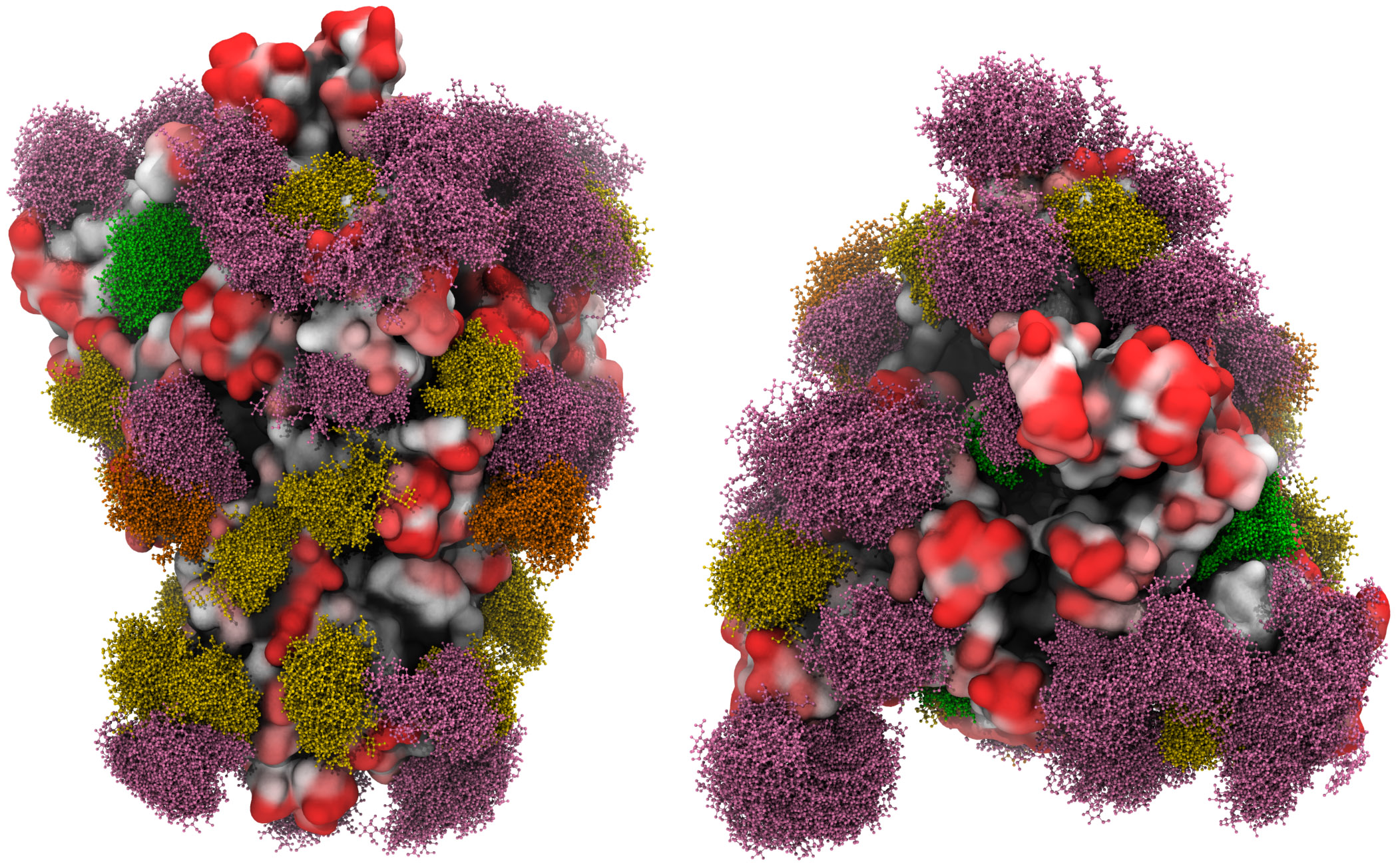
Three-dimensional molecular simulation of the spike glycoprotein with the moss effect showing the glycan shielding [Grant et al., 2020].
It is no coincidence that memory CD4 TH & CD8 TC cells – both TEM and TCM – gained and subsequently conserved from previous exposure to other common cold-causing coronaviruses, target SARS-CoV-2 nsps 7 & 13 and the structural nuclesocapsid protein.
SARS-CoV-2-specific function of IgA.
SARS-CoV-2’s infection cycle is approximately two weeks, as we set out in April 2020, with this period reflecting both viral pathogenesis and any disease progression:
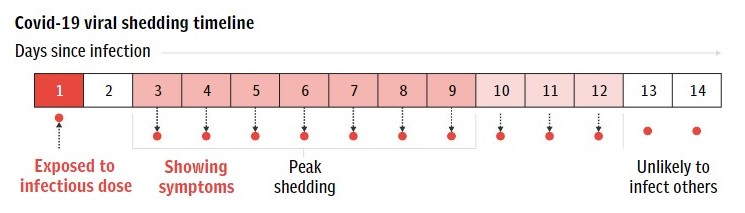
Week one corresponds to viral infection and replication. It also includes peak viremia or viral shedding. 99.6% of those who get SARS-CoV-2 are moving toward viral clearance by the end of week one, as the innate immune response has overcome the infection.
Week two corresponds to disease progression if the infection has moved from upper to lower respiratory tract. Here it can bind to alveolar macrophages and pneumocytes, causing tissue damage to the lungs and leading to pulmonary complications and secondary infections, such as viral and bacterial pneumonia.
This highlights the overriding objective of overcoming infection in week one and therefore the crucial importance of the speed of immune response. While the innate immune response is near instantaneous, the adaptive immune response needs time to program and activate the antigen-specific response, known as seroconversion. The quicker seroconversion occurs, the quicker antigen-specific antibodies are in circulation in the humoral system.
As the first seven days are key, then so is the speed of seroconversion.
Yu et al. [2020] show that following expression of SARS-CoV-2 symptoms, i.e. 3 days following primary infection, IgM and IgG seroconversion takes 5 days. However, IgA seroconversion takes 2 days. IgA is effective 3 days sooner than IgG.
They also show that IgM titers do not increase in line with disease severity and that IgM titers are lower than IgA regardless of disease severity. This means that IgM’s efficacy as an antibody decreases with disease severity and that IgM is less effective than IgA, even though IgM is the adaptive immune system’s ‘first-responder’ antibody. IgA was also the only antibody to show a positive correlation with disease severity (based upon critically ill patients quantified by APACHE-II scoring).
Conclusions.
The spike protein is not an effective target for viral countermeasures, as we have explained previously here. Vaccine and antiviral candidates that aim to stimulate IgG only ignore both the respiratory tract and IgA, as we have explained previously. The key region is the upper respiratory tract and the key antibody is IgA in general and subclass IgA2 – or secretory IgA – in particular.
- IgA can induce the release of interleukin-6 and 10 cytokines. Interleukin-6 can be used as a indicator of COVID-19 disease severity: using a threshold of 43(24.3-80)pg/ml [Yong et al.; Giofoni et al.; Herold et al.] to identify disease severity upon hospitalisation would both save lives and have saved lives, many thousands of lives.
Interleukin-10 can modulate isotype class switching and thereby increase the effectiveness of the adaptive immune response by switching antibodies to the isotype deemed most effective.
- IgA1 has a more flexible hinge structure and Fab arrangement (Fab-Fab centre separation of 17nm compared to IgG Fab-Fab centre separation of 7-9nm, [Boehm et al., 1999]) and IgA2 has glycosylation of its hinge region that provides it with greater binding affinity to SARS-CoV-2 spike protein trimers.
This shows that IgA is more structurally responsive to SARS-CoV-2’s morphology and phylogenetic antigen shift.
- IgA antibodies express chemokine receptor CCR10, the ligand of which, CCL28, is expressed on alvelolar epithelial cells. These are the cells at risk in week two if infection spreads to the lower respiratory tract. So IgA is also forward-planning by migrating toward cells that may be at risk in the event of disease progression.
- In respect of SARS-CoV-2, IgA not IgM should be considered as the first-responder antibody due to its quicker seroconversion. Given the high significance of week one of the infection period, this is significant and reinforces the importance of IgA in early treatment of SARS-CoV-2 both to accelerate viral clearance and prevent disease progression.
- Developing B cells or plasmablasts secrete IgA in greater proportions than IgM and IgG, with an IgA:IgG ratio of 2.2:1 [Sterlin et al.]
- IgA1 functions alongside IgA2, with IgA1 providing neutralising immunity while IgA2 provides protective or sterilising immunity. Sterlin et al. substantiate Wang et al.’s study that IgA1 is far more effective than IgG (Sterlin et al. 7x; Wang et al. 7.5x) in neutralising SARS-CoV-2. Again, this is particularly relevant in the early stages of infection, so the crucial week one.
- IgA is a stronger but shorter-lived antibody response to SARS-CoV-2 than both IgM and IgG. However, as the key period is only seven days – week one following infection – this is not an issue as IgA is effective for up to four weeks.
- IgA can provide sterilising or protective immunity, thereby preventing an individual from catching and spreading SARS-CoV-2. IgG cannot.
IgA is is both the fastest and most effective SARS-CoV-2-specific antibody. It also increases production in response to disease severity. Why is it effectively ignored in favour of IgG stimulation, an antibody that is less effective, not as strong and takes longer for seroconversion?