Peak Infections And Peak Deaths.
COVID-19 deaths peaked in the UK on 8th April 2020, one year ago today. This followed peak infections on 19th March 2020, a little under three weeks previous, in line with SARS-CoV-2’s infection cycle of two weeks. Week one occurs in the upper respiratory tract and includes exposure, cellular fusion & entry, viral replication and viral shedding. Peak viremia also occurs within week one. For 99.6% of individuals, by the end of week one the innate immune response – aided by any adaptive immune response from previous exposure to other common-cold causing coronaviruses – has overcome viral infection and the individual is moving toward viral clearance. Week two occurs in the lower respiratory tract, if the virus has spread as a result of high viral load in week one overwhelming the immune system or existing comorbidities, especially those related to the disfunction in the renin-angiotensin system.
We first highlighted this infection cycle in early April 2020, over one year ago and within days of peak deaths. With SARS-CoV-2 source genome NC_045512.2 having been fully mapped in January 2020, it was clear by March that SARS-CoV-2 was a seasonal irritant and that it was most certainly not the killer virus of death. As we set out later in April 2020, this was a key determinant in Public Health England’ and the Advisory Committee on Dangerous Pathogens’ decision to downgrade SARS-CoV-2 from high consequence infectious disease on 19th March 2020, before the first lockdown was imposed.
In late March 2020, the Evolutionary Ecology of Infectious Disease laboratory, part of Oxford University Department of Zoology, published hyper-accurate and near real-time data on SARS-CoV-2 viral infection, gathered from frontline observation in the UK and Italy. The study showed that at least 68% and as high as 80% of the United Kingdom population had been exposed to SARS-CoV-2 by 19th March 2020.
In September 2020, our subsequent research identified a timeline for SARS-CoV-2 that suggests a recombination with lineage A sarbecovirus beta genus coronavirus HCoV-OC43 around 2013/14. This led to our positing of two connected hypotheses in November 2020, extracted summaries of which are;
Hypothesis 1 – SARS-CoV-2 has been around for several years.
You can discount SARS-CoV as that stopped being reported in 2004 and was very localised in its nature with distinct symptoms and much higher mortality rate. Likewise MERS-CoV on account of the same two reasons. As we referenced back in August, one of the principal mistakes made early on was the nomenclature of SARS-CoV-2 when it has turned out to be neither severe nor acute but where by making it sound like a re-run of SARS-CoV, it made it out to be far more dangerous than it was or is. So you are left with HCoV-229E; HCoV-NL63; HCoV-HKU1 and HCoV-OC43 – the four coronaviruses that cause the common cold.
Except the common cold is dealt with by the innate immune system so there would not be any antigen-specific memory T cells in existence.
SARS-CoV-2 is classified as a sarbecovirus lineage beta genus coronavirus but we’ve already ruled out SARS-CoV (the only other pathogenic sarbecovirus). You can rule out the alphas as SARS-CoV-2 is a beta genus plus the fact that neither HCoV-229E nor HCoV-NL63 have a furin cleavage site. Rule out the other two beta genus as they are dealt with by the innate immune system – as mentioned above – and you are left with the fact that the proliferated T cells are SARS-CoV-2-specfic and the individuals had previous primary infection, some time before SARS-CoV-2 but before it was designated as such.
That primary infection caused the subsequent conservation of memory T cells which have proliferated upon secondary infection (in 2020), which is the very nature of immunological memory and immunity.
Under Hypothesis 1, SARS-CoV-2 has been around for a number of years, infecting individuals along the way and providing a significant proportion of them with immunity. Those without T cell proliferation dealt with the infection by innate immune response only.
With research proving that memory T cells for a fellow sarbecovirus can last anything from 6 – 17 years (usually limited only by the period of observation) and allowing for the homology between SARS-CoV and SARS-CoV-2 in terms of their nsp7, nsp13 and nucleocapsid sequences, long-term immunity through memory T cells can occur.
Hypothesis 2 – Previous Exposure To Another Coronavirus Can Start Immunity.
Primary infection with one of the main four pathogenic coronaviruses – most likely beta genus HCov-HKU1 or HCoV-OC43, less likely alpha genus HCoV-229E – causes the conservation of memory T cells which then proliferate upon exposure to SARS-CoV-2, as a result of the homology of any/all of the respective nsp7, nsp13 and nucleocapsid proteins.
The level of homology is lower and may be sufficient only to partially arm an adaptive immune response. A full antigen-specific response is not required because by the time the adaptive immune system would be ready to commence its response, the infection has already been overcome by the innate response. However, elements of the virus’ genetic sequence are retained by memory T cells, with both TH & TC cells proliferating upon primary infection with SARS-CoV-2 but which the immunological memory believes to be secondary infection.
Under Hypothesis 2, something as simple as catching a cold may kick start immunity against subsequent SARS-CoV-2 infection, by creating memory T cells that have not encountered SARS-CoV-2 but which react to it if they do.
Persistent Antigen Exposure – Immunity Through Exposure To Other Viruses.
Hypothesis 2 is an area we have researched subsequently in greater detail, as the data supports the view that persistent antigen exposure to other coronaviruses increases SARS-CoV-2 immunity.
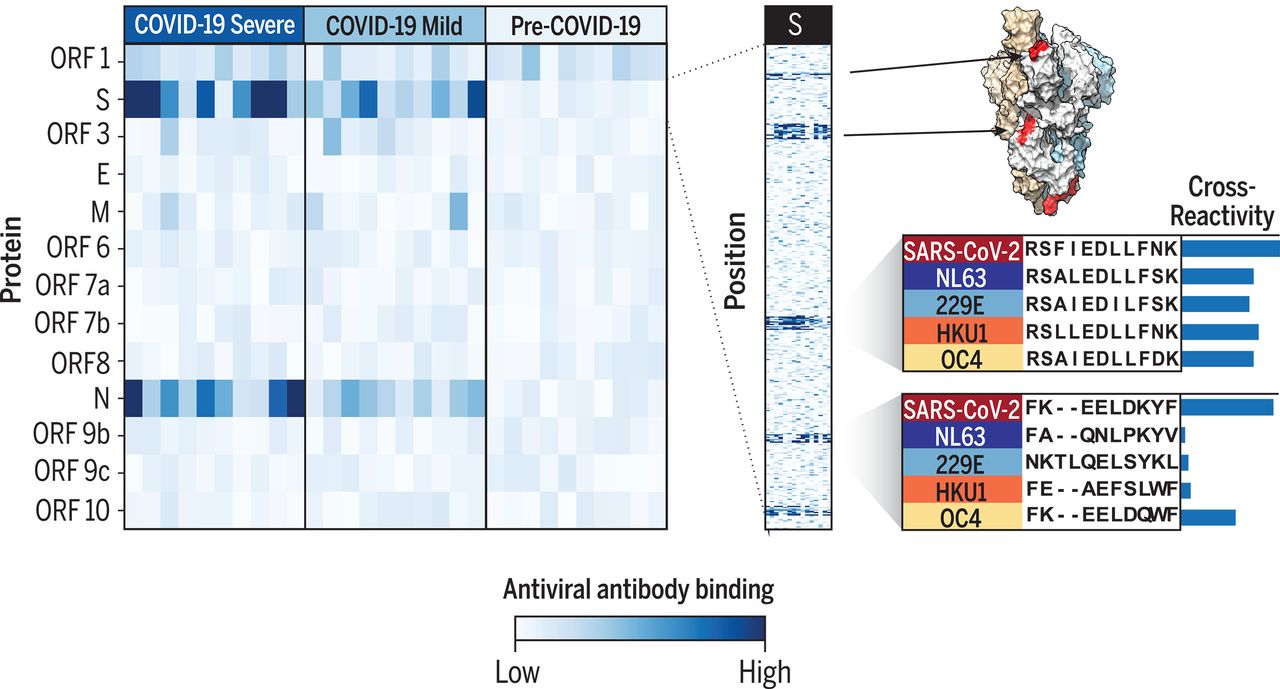
Cross-reactive epitopes of SARS-CoV-2 and the other four common-cold causing coronaviruses [Shrock et al., 2020].
It applies not just to common cold-causing coronaviruses but also to common cold-causing rhinoviruses, with the latter shown by the University of Glasgow Centre for Virus Research (CVR) in their recent research, as we explained at the end of last month.
Persistent antigen exposure is regular, low dosage exposure, the kind you would get through work and social activities, such as shopping, going to a restaurant or meeting friends. Persistent antigen exposure is why countries without developed healthcare systems and advanced medications have such low COVID-19 mortality rates. We calculated the truly terrifying nature of the NHS clinical response compared to the rest of the world back in January, based upon the prevailing data and the results can be read here.
These countries also do not have the NHS, an organisation that has not only failed spectacularly to prevent the deaths of those presenting with moderate to high disease severity but also has caused the deaths of tens of thousands through facilitating disease progression. The sick went into hospital where they got sicker and died as a result of the NHS clinical response, which has been medieval in its effectiveness.
What Would We Have Done Differently?
In April 2020, having assessed source genome NC_045512.2, understanding its pathogenesis as well as interaction with the immune system, we estimated that 20,000-25,000 would die. Slightly more than the annual deaths from seasonal/winter flu but slightly less than the annual excess winter deaths. Applying the worldwide average mortality rate, UK COVID-19 deaths would be 25,225. So, one year on, we were accurate, one could say very accurate.
Certainly somewhat more accurate than the ridiculous fantasy predictions of Neil Ferguson, whose irrealis mood and conditional voice was speculative science fiction at its worst: ‘up to 510,000 could die’. In contrast, we used the realis mood and indicative voice: 20,000-25,000 will die. As always, you can read more of Neil Ferguson’s comedy predictions and epic fails here, when we first highlighted them in April 2020.
- Administered high dosage calcifediol or similar upon hospitalisation due to disease severity.
Vitamin D has been proven over and over both to prevent viral infection and to reduce disease severity and prevent disease progression. We first identified the crucial role of vitamin D in July 2020 and expanded upon this in October 2020, with other groups around the world also proving its efficacy. Nogués et al. show that for those requiring hospitalisation due to COVID-19 disease severity, treatment upon admission with calcifediol reduces subsequent transfer to intensive care from 21% to 5.4% and reduces mortality from admission from 15% to 6.5%. This equates to a 57% reduction in mortality rate in those with moderate to high COVID-19 disease severity.
This measure alone would have saved 71,942 lives in the UK.
- Provided oxygen concentrators and installed oxygen generators.
Ventilators were never required in the quantities implied by the government and NHS. Too many were ordered and not required, a significant number of which were supplied at hugely-inflated prices under contracts awarded to chums of politicians and ministers. In addition, there was a shortage of medical oxygen as only a very small number of NHS hospitals possessed oxygen generators and were therefore able to generate their own supply.
An Inmatec medical oxygen generator.
Non-invasive rather than invasive oxygen support would have been a far more effective focus, looking at low/high flow oxygen and non-invasive oxygen support as the principal means of delivery. Home oxygen concentrators were not freely available as if they had been, more individuals in high risk groups could have been kept away from NHS hospitals, where they were many times more likely to suffer an increase in COVID-19 disease severity and die. It is noteworthy that Susan Hill, chief scientific officer for NHS England, on 2nd April 2020 specifically prohibited NHS Trusts and clinical commissioning groups from requesting home oxygen concentrators.
Front line clinicians had identified the benefits of concentrators in increasing oxygen saturation, especially where a Trust had no capacity for on-site generation. Preventing Trusts from accessing non-invasive oxygen delivery systems (remember that the NHS was promised every resource it needed) cost lives.
With the useless, pointless track & trace programme costing £22 billion (and counting), it would have far better to spend some of this sum on properly-equipping all NHS Trusts with their own on-site oxygen generators, as well as ensuring the most commonly-used methods of non-invasive oxygen administration were freely accessible and available.
A medical oxygen generator with a production capacity of 15 Nm3/h at 95% purity costs a little over £24,000 (that’s the retail cost for just one, not what the NHS would pay for thousands unless the contract was awarded to a chum of Boris Johnson or Matt Hancock). Therefore, with 223 NHS Trusts in the UK (source: The King’s Fund), each one could be given four generators at a total retail cost of £21.4 million. That’s 0.1% of the cost of the complete waste of money that is track & trace, for which every NHS Trust in the UK would have its own state-of-the-art on-site oxygen generation. Which would save more lives?
- Used interleukin-6 as an indicator of COVID-19 disease severity.
Interleukin-6 is a cytokine released in response to invasive infection. There is widespread data showing interleukin-6 levels can be used to identify those with moderate to high level COVID-19 disease severity where a clinical response can attenuate disease progression and severity.
- Focused upon the secondary infections and conditions presented where SARS-CoV-2 is the causative agent.
Instead, the NHS clinical response blindly focused upon RT-PCR testing and viewing SARS-CoV-2 as some new chimeric illness with previously unknown and apparently untreatable symptoms. If in week two of its infection cycle SARS-CoV-2 spreads to the lower respiratory tract, damaging alveolar macrophges and pneumocytes, it can cause tissue damage and increase the risk of secondary infection through viral or bacterial pneumonia. In the same way as other respiratory viruses such as influenza A. High viral load can also cause cytokine storm, triggering systemic inflammatory response syndrome (SIRS); compensatory anti-inflammatory response syndrome (CARS) and acute respiratory distress syndrome (ARDS).
The NHS became paralysed by the ‘killer virus of death’ when it should have been looking for eminently treatable, well-known symptoms. ‘Treat what you see’ would have identified more cases of viral/bacterial pneumonia and SIRS/CARS/ARDS.
Lives would have been lost but lives are lost every year to seasonal/winter flu and to excess winter deaths. Approximately 48,000 lives are lost annually in the UK to sepsis. However, far fewer lives would have been lost: more than 70,000 lives would have been saved had the government and NHS listened to people who knew what they were talking about.
Twelve months on from peak deaths, the individuals in charge – Matt Hancock, Chris Witty, Boris Johnson, Nadhim Zahawi – have absolutely no idea what they are doing or what they are talking about. They are responsible now for the avoidable and unnecessary deaths of over 100,000 people, let alone the personal; professional; financial; economic; academic and mental misery inflicted on tens of millions of people.