UK COVID-19 mortality rate remains one of the highest in the world.
On a population-adjusted basis (for fair comparison) the UK mortality rate is 4.36x the worldwide average, which means there have been an additional 98,364 deaths in the UK (@0500UTC 13/05/21, source: Johns Hopkins Coronavirus Resource Center/Worldmeters). Deaths that were avoidable. One of the key reasons for the completely unacceptable and unnecessary total number of deaths is the NHS clinical response. Cheap, simple tests that save lives were ignored.
Noone should die of COVID-19 per se. Certain groups are at greater or high risk, such as the frail as a result of immunosenescence and those with comorbidities, principally arising from Western diet-induced comorbidities causing dysfunction of their renin-angiotensin system. However, as a respiratory virus with pathogenesis focused in the upper respiratory tract and a member of the coronaviridae family (meaning the immune system has 10,000 years’ experience in recognising & fighting it, over 7,160 years of those with the beta genus) it is not – and never was – the killer virus of death as portrayed by the UK government and public health professionals.
As we highlighted in February, individuals supposedly in charge such as Matt Hancock and Chris Witty failed to understand the difference between SARS-CoV binding in the lower respiratory tract and SARS-CoV-2 binding in the upper respiratory tract as a result of its greater affinity for TMPRSS2. As we explained in January, the same individuals have also deliberately confused ‘infectiousness’ and ‘infectivity’ in their attempts to lie their way out of their mistakes.
If SARS-CoV-2 therefore isn’t the killer virus of death that those in charge want everyone to believe, why have so many died?
As early as July 2020 and October 2020 we had set out the importance of the vitamin D pathways in providing viral immunity and preventing disease progression. Nitric oxide in the upper respiratory tract prevents viral infection and high dosage calcifediol upon hospital admission reduces disease progression after admission by 74% and mortality by 57% [Nogués et al.].
The focus of this study is on the NHS’ failure to identify viral load and/or disease progression in those hospitalised.
High viral load in the early stages of infection can trigger cytokine release storm or cytokine storm, which is the excessive release of inflammatory ctyokines. This can lead to systemic inflammatory response syndrome (SIRS), the counter-function compensatory anti-inflammatory response syndrome (CARS) and acute respiratory distress syndrome (ARDS). We first identified the key role of cytokine storm in progressing COVID-19 disease severity in April 2020, over one year ago. Cytokine storm mediates septic shock and sepsis is one of the NHS’ greatest blinds spots, with sepsis accounting for 48,000 deaths annually in the UK. If the NHS knew how to spot the symptoms of sepsis and test for it (as set out later, it is not difficult), tens of thousands of lives would be saved every year. The parallel with its inability to treat COVID-19 effectively is all too stark.
SARS-CoV-2 also becomes dangerous when high viral load accumulated in the upper respiratory tract overwhelms the innate system’s capacity in week one of the infection cycle and causes the virus to spread to the lower respiratory tract in week two of the infection cycle (the point at which 99.4% of those infected are moving toward viral clearance having overcome infection). In the lower respiratory tract damage is done to alveolar macrophages and pneumocytes, damaging the lungs, which exacerbates dyspnea (respiratory distress). Damage in the lower respiratory tract also mediates viral and bacterial pneumonia which, if undetected or not treated, can be fatal.
Viral/bacterial pneumonia and cytokine storm account for the vast majority of COVID-19 related deaths.
The Flawed Obsession With RT-PCR Testing.
The hysteria surrounding SARS-CoV-2 meant that the sole focus was upon ‘testing for the killer virus of death’ using nucleic acid/RT-PCR testing. We first outlined the inappropriate nature of nucleic acid testing in March 2020, fifteen months ago. There are more detailed evaluations of why you cannot reply upon RT-PCR testing for just about anything, from August 2020 and September 2020. There has been an obsession with the binary outcomes of a testing method that, as a result of the homology of coronaviruses’ antigen peptide chains, is just as likely to pick up the common cold (a false positive) or that, through antigen shift from amino acid substitutions, SNPs and indels, is just as likely to miss it (a false negative).
Test For C-Reactive Protein, Procalitonin And Interleukin 6.
If you want to perform tests that have some beneficial outcome to the patient, test for C-reactive protein (CRP); procalcitonin (PCT*) and interleukin 6 (IL-6). Each of these, whether independently or combined, are indicators of COVID-19 disease progression and disease severity.
*not to be confused with PCR/RT-PCR, the method of nucleic acid testing.
CRP.
CRP is a protein found in the blood. It is a pattern recognition receptor that forms part of the early-warning detection system in the innate immune system. It assists with the destruction by phagocytosis of infected/dead cells by signalling their location to other cells. CRP itself is triggered by the release of interleukin 6 (explained below).
A normal CRP level would be 0.5 – 3 mg/l. This level can rise in those with chronic cardiovascular conditions but by small amounts, to the degree that someone with a CRP level of 4 mg/l could be considered as at higher risk of diabetes or heart disease. However, in response to infection the CRP level rises rapidly and substantially.
Ahnach et al. [2020] show in their study of 145 patients hospitalised with COVID-19 disease progression, a median CRP level of 7.7 mg/l upon admission. In those who progressed to severe disease severity, the median CRP level increased to 86.4 mg/l (with the range being 21.69 – 145.8). Ahnach concludes “CRP was a robust predictor of adverse disease outcome.”. Hesse et al. [2020] show in their study of 12,270 patients with SARS-CoV-2, a median CRP level of 115 mg/l in those without COVID-19 disease progression and 136 mg/l in those with severe disease progression.
PCT.
Procalcitonin is a hormone that is used in the modulation of calcium levels in the blood. It is created and then converted into calcitonin in the thyroid meaning that there should be very low levels of it left in a healthy individual. Normally it is below the threshold for standard detection, deemed to be <0.01 µg/l. However, in response to infection – and in particular bacterial infection – its production increases as it is triggered by inflammatory infection.
Hesse et al. show a median PCT level of 0.25 µg/l in those with SARS-CoV-2 infection but no COVID-19 disease progression and 2.1 µg/l in those with severe disease progression. A 25-fold increase in PCT level as a marker of potential disease progression is a clear and robust analogue, even more so a 210-fold increase as a marker for severe disease severity.
IL-6.
Interleukin 6 is a cytokine involved in the innate immune system. It performs a number of functions, including being a key signaller in pyrexia (fever) to fight infection, something we explain here. Its release by leukocytes in the early stages of an innate immune response and the relevance of excessive cytokine release as the trigger for cytokine storm should have made it a key biomarker of viral load and disease progression. We first identified this function in January 2021 and again last month.
A normal level of IL-6 in a healthy individual would be in the range 5 – 15 pg/ml. Hesse et al. show a median IL-6 level of 44.4 pg/ml in those with SARS-CoV-2 infection but no COVID-19 disease progression and 503.8 pg/ml in those with severe disease progression. Using 10 pg/ml as a baseline, the 4-fold to 50-fold increase in median level of IL-6 through disease progression shows it is a clear and robust analogue.
The highest value in Hesse et al.’s study is 987 pg/ml. This is substantiated by Sun et al. [2020]’s study that shows a high correlation between IL-6 levels and COVID-19 disease severity and mortality.
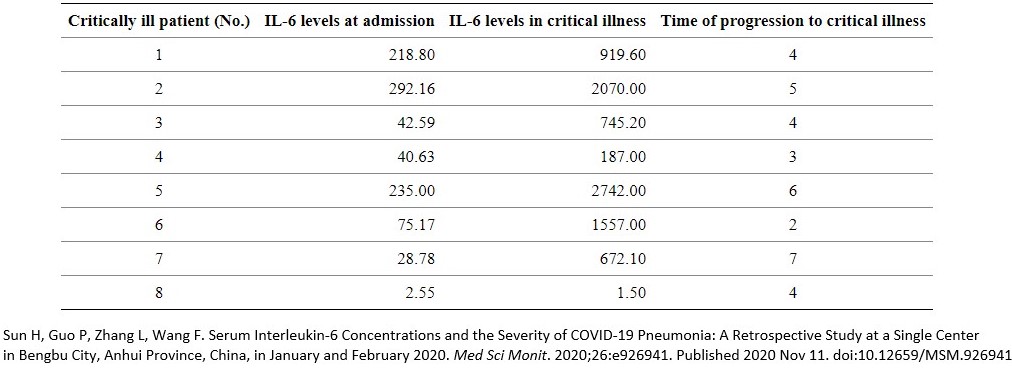
Their observations include; “Several retrospective studies have shown that increased levels of IL-6 are associated with death in patients with severe COVID-19 infection…Elevated IL-6 is also associated with disease severity and course, suggesting that this cytokine may be a marker for disease monitoring in patients with severe COVID-19” and “Serum concentrations of IL-6 and C-reactive protein (CRP) can effectively assess disease severity, suggesting that IL-6 and CRP may be independent factors predictive of the severity of COVID-19.”
Bearing in mind that bacterial/viral pneumonia is one of the two main causes of death as secondary infections mediated by COVID-19 disease progression, one would pay significant attention to Sun et al.’s observation that interleukin 6 “is highly significant in the differential diagnosis of bacterial and viral infections.” They conclude:
“Increased levels of IL-6 and CRP were found to be predictive of the need for mechanical ventilation, indicating that measurement of IL-6 can guide the escalation of treatment in patients with COVID-19 – related hyperinflammatory syndrome. Taken together, these findings suggested that monitoring serum concentrations of IL-6 may be crucial for identifying disease progression in patients infected with SARS-CoV-2.“
Conclusions.
Bacterial and viral pneumonia and cytokine storm (SIRS/CARS/ARDS) are the principal causes of death linked to COVID-19. Being able to identify these conditions within any COVID-19 disease progression and severity saves lives.
CRP, PCT and IL-6 are biomarkers of COVID-19 severity and they can be used as predictors of disease progression with PCT having particular relevance to bacterial pneumonia and IL-6 to cytokine storm.
Their results can be used to allocate available resources efficiently, for example an IL-6 level of 35 pg/ml that is static suggests little need for invasive oxygen assistance compared to a level of 30 pg/ml upon admission that has risen to 125 pg/ml and is still rising.
CRP, PCT and IL-6 should have been the default tests to identify disease progression and severity as they are patient-specific, thereby reflecting the host:virus interaction. The cult-like focus upon RT-PCR is pointless as it is a one-size fits all approach that is backward looking and wildly inaccurate. In the above IL-6 example, the individual has SARS-CoV-2 infection upon admission and after admission: the binary outcome is unchanged because RT-PCR testing is a polar indicator with only positive/negative outcomes (which are more often than not wrong anyway). Progressive indicators that show the degree of infection and the direction of travel of any disease severity, e.g. ‘is this person getting better or worse?’ are far more useful.
Other countries’ healthcare systems were adopting these methods of testing as early as February 2020. For some reason the NHS completely ignored them.
Our findings are reflected by Tan et al. [2020] who validate the role of these biomarkers. Their evaluation confirms that CRP, PCT and IL-6 each differentiate between COVID-19 moderate/severe and critical disease severity.
These three factors can be measured by cheap, simple tests. Cheap, simple tests that are effective at indicating those at the greatest risk of disease progression and severity. £22 billion – and counting – has been wasted on a ‘track & trace’ program that doesn’t work and is not needed. As we set out in April, every NHS Trust could have been four oxygen generators at a total cost of 0.1% of the gargantuan waste of money that is ‘track & trace’. If the cost of CRP/PCT/IL-6 testing was a maximum of £50 for each of those 98,364 unnecessary excess deaths, it would have cost just £4.91 million or only another 0.02% of that £22 billion waste.
If that were not enough, those tests if adopted and implemented on a default basis would also prevent thousands of deaths from sepsis annually.