‘The Ships Hung In The Sky In Much The Same Way That Bricks Don’t.’
The above is a line from Douglas Adams’ The Hitchhiker’s Guide To The Galaxy, referring to the arrival of the Vogon Constructor Fleet. The relevance to SARS-CoV-2 is that even a brick if thrown is airborne spread…for a very short time. It is not however airborne per se.
A virus can spread in one or more ways as we listed in March 2020. SARS-CoV-2 virions are droplet spread, in that they are exhaled within sputum or mucal ejecta. If that substance is then transferred to, say, a door handle then it is possible for it to be transferred via that surface (known as a fomite) but only for a limited period of time, based upon the virion’s T1/2 on that particular surface. In general SARS-CoV-2 remains infectious on fomites, on a TCID50 basis, for up to 5-7 hours, as we explained first in April 2020 and expanded upon in December 2020. Touching a fomite that carries more than a minimum infectious dose of SARS-CoV-2 – generally accepted to be ~200 virions – can increase the risk of infection if that individual then transfers the sputum/mucal ejecta to their nose but this is not contact spread. Touching an infected surface is different to contact spread, again the list of main methods is set out here.
For SARS-CoV-2 to be airborne spread, imagine you are standing on one side of the road and I am standing on the other, say 50 feet apart: you put a stone in your outstretched hand. That stone must be able to travel from you to me without external stimulus. And if infectious, stones in sufficient numbers to exceed a minimum infectious dose. Yet SARS-CoV-2’s structure has no means to allow it to be carried on the wind. An additional, immediate observation is that as other coronaviridae viruses are not airborne spread why should SARS-CoV-2 be any different?
However, as the heading infers, there is a difference between passing through the air and being airborne. Again, a brick passes through the air after being propelled but it quickly falls to the ground through gravity. SARS-CoV-2 is no different.
A SARS-CoV-2 virion is 0.1-0.12 um or microns in diameter. The first point to highlight here is that dedicated surgical masks, certified to FFP2/N95 standards, only filter out particles >0.3 microns in diameter, so it is easy to work out just how ineffective a piece of material is at preventing viral entry. What a non-surgical face covering will do when strapped over the wearer’s respiratory system for hours/days on end is ensure re-inhalation of any infected sputum/mucal ejecta, meaning the wearer will keep re-breathing their own infection. This will increase viral load which leads to COVID-19 disease progression & severity, compared to moving toward viral clearance that would be achieved through normal, unconstrained exhalation. We first highlighted this in September 2020 and the enforced mass wearing of non-surgical face coverings is one of the three main reasons that the UK government response has caused tens of thousands of unnecessary, avoidable deaths.
The newly-replicated virions are exhaled in droplets of sputum or mucal ejecta and it is the properties of these droplets not SARS-CoV-2 virions that are the key to whether or not it is airborne spread.
Droplets vs Aerosols.
All manner of things come out of your mouth: in speaking, laughing, coughing, vomiting, sneezing and exhaling, you emit respiratory particles in the range 0.05 to 500 microns. These exhaled respiratory particles are categorised either as droplets or aerosols, depending upon their size.
Larger particles are droplets and smaller particles are aerosols, although there is no standardised measure to determine each: the cutoff lies anywhere between 5 microns and 20 microns. An important qualifying factor that does narrow the cutoff point is that aerosols should be able to be inhaled and reach the lower respiratory tract, whereas droplets are too large to go further than the upper respiratory tract. This has particular relevance to SARS-CoV-2 given that ground zero for any COVID-19 disease severity is through binding to alveolar macrophages and pneumocytes in the lower respiratory tract, during week two of the infection cycle.
Another indicator is that droplet spread is caused through coughing, sneezing and talking. In this respect perspex screens and visors are very effective as any infected droplets are caught on whichever side of the screen or visor, preventing person-to-person transmission. With a visor, the wearer’s respiratory system is not constricted and they are moving toward viral clearance by exhaling any newly-replicated virions rather than re-inhaling them over & over, as would be the case with a non-surgical face covering.
Particles larger than 1 micron become subject to gravity [Cox and Wathes, 1995] and will fall to the ground upon exhalation. Stokes Law comes into play, determining the trajectory and velocity of the fall, especially when sneezed or coughed out. The concept of social distancing is rooted in Wells’ interpretation [1934] of Stokes Law. Given it is now over 85 years old, this work shows the constant, repeatable ways in which respiratory particles can carry or spread a pathogen.
Also, upon exhalation all respiratory particles become subject to environmental factors, such as thermal variation, turbulence and electrostatic charge, as well the physical aspects of their own Brownian motion and inertia.
We identified in July 2020 that SARS-CoV-2 inactivates when the ambient temperature rises above 20’c, with Uddin et al. [2020] concurring in October 2020. Jayaweera et al. [2020] conclude that; “Viruses in aerosols lose or gain the viability and infectivity because of environmental stresses caused by temperature, relative humidity, and sunlight before they reach a susceptible host.”
Evaporation Upon Exhalation Turns Particles Into Residue.
The net result of all these factors is that upon exhalation, respiratory particles will immediately begin to evaporate, shrinking in diameter by half. The particle then becomes non-volatile, dehydrated residue, which may contain newly-replicated virions with two factors to consider:
Firstly the larger the particle, i.e. droplets (so immediately we can rule out aerosols), the greater the number of virions within it. Secondly, the loss of volume of the residue and its spread pattern, e.g. whether a cough or adherence to a fomite, increases the distribution of virions throughout the residue. This means that virions will not be present throughout the residue and varying proportions of residue will either contain virions or be blank, i.e. contain no virions. [Fuchs and Sutugin, 1966; Raabe, 1968; Zuo et al., 2013; Alonso et al., 2015; Fernandes et al., 2019; Anand and Mayya, 2020]. Anand and Mayya observe that a “significant part of the ejected droplets would dry up to form blank residues carrying no RNA copies, thereby becoming unviable and harmless from the point of view of infection transfer.“
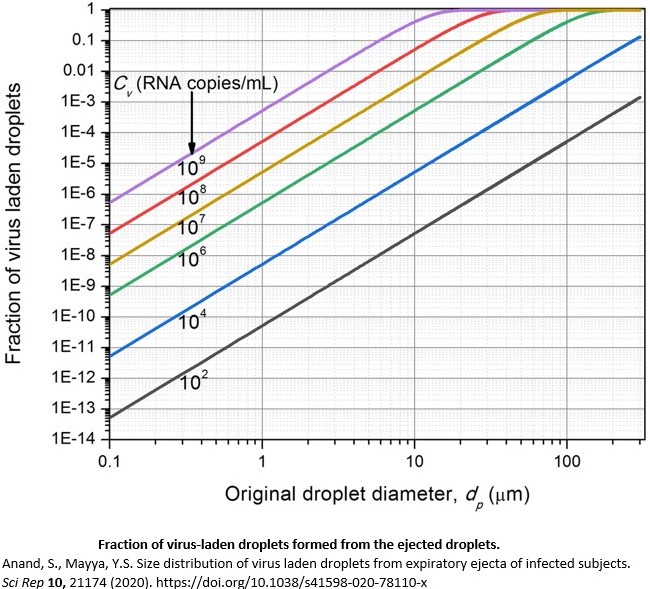
Using the upper range value of 20 microns as the aerosol/droplet cutoff, the distribution of virions is brought into greater focus by Stadnytskyi et al. [2020] who calculate that at moderate viral load, a maximum of 0.37% of residue will carry any virion(s), i.e. ≥99.96% of residue is blank and does not carry any virion(s). In other words, 99.9% of aerosol respiratory particles are not carrying any virions, both at the point of exhalation and subsequent conversion to aerosol residue. This is substantiated by Anand and Mayya who calculate that at up to moderate viral load particles “less than 20 µm [20 microns] are unlikely to carry any viral load.” They conclude that “In real indoor scenario, this would amount to risk of inhaling less than one virus carrying droplet if a person stays for an hour in the room with the infected person.“
Aerosol particles even of this size cannot reach the lower respiratory tract anyway so it is not possible for SARS-CoV-2 to reach the lower respiratory tract – and there cause COVID-19 disease progression and any severity – through airborne transmission.
Duguid [1945] established 75 years ago the inverse relationship between oral and nasal respiration: breathing through the mouth you exhale more aerosols than droplets whereas through the nose you exhale more droplets than aerosols. This is relevant as breathing through the nose stimulates the production of nitric oxide – the most effective killer of SARS-CoV-2 in the upper respiratory tract before it replicates – and this has formed a constant part of our How To Stay Safe By Not Following Government Advice guidelines on SARS-CoV-2 after we first highlighted its significance in October 2020.
Anand and Mayya show further that in those with up to moderate viral load, the respiratory particles will not carry sufficient virions to constitute a minimum infectious dose, i.e. sufficient to infect 50% of those exposed. This is very significant as our view has always been that SARS-CoV-2 is all about viral load in the upper respiratory tract: you want to avoid accumulating viral load (lockdown and wearing non-surgical face coverings both increase viral load) and their findings show that viral load also determines transmission. The degree of infectiousness, e.g. whether B1.17 may be more infectious than B1.617 which may more infectious than B1.1.298, is irrelevant if SARS-CoV-2 cannot be transmitted in a low viral load.
As a final point, there is no evidence to support the stance that droplet spread outbreaks of any pathogen are more serious (greater infectivity) than airborne spread outbreaks. Indeed Shiu et al. [2019] prove the opposite, reinforcing the position that aerosol particles carry fewer virions and are inactivated more through dehydration and environment. In other words if a virus is now supposed to be airborne spread, that means it has lower infectivity.
Conclusions.
- SARS-CoV-2 is droplet spread through respiratory particles of sputum and mucal ejecta. The volume and size of these particles is linked to the individual’s viral load.
- Viral load is of even greater significance as it mediates viral infection, disease progression & severity and viral transmission.
- Droplets fall to the ground within 1.5-2 metres as a result of gravity. Through direct inhalation or via a fomite, these droplets can transmit SARS-CoV-2.
- Upon exhalation, all respiratory particles begin to evaporate and shrink in diameter and volume. Those light enough to escape gravity (<1 micron) become dehydrated aerosol residue. Any virions contained in this residue have a T1/2 of ~1 hour, so are no longer infectious after this time.
- At up to moderate viral load, 99.9% of aerosol residue particles do not contain virions so pose no infection risk and 99.9% of droplet particles up to 20 microns do not contain virions so pose no infection risk.
- Droplet particles large enough to pose an infection risk are subject to gravity and fall to the ground upon exhalation. Particles small enough to become aerosol residue either contain no virions or insufficient virions to pose an infection risk.
- If a respiratory particle is large enough to carry virions it is too large to reach the lower respiratory tract but may cause infection in the upper respiratory tract, i.e. droplet spread.
- Therefore, SARS-CoV-2 is not airborne spread as defined by the established, acknowledged definition of viral transmission. Aerosol residue can pass through air but the distribution of virions within aerosol residue mean it does not pose an infection risk.