UK COVID-19 Mortality Rate.
The most straightforward, simple and transparent measure of whether non-surgical face coverings work is that even now, over 18 months into the current insanity, the UK’s COVID-19 mortality rate is 3.27-times higher than the worldwide average (@0500UTC today, source: Johns Hopkins Coronavirus Resource Center/Worldmeters). With the worldwide average being just what its name infers – comprising 221 countries and territories plus two merchant vessels – it can be used as a comprehensive and fair baseline for comparison. The 3.27-fold higher mortality rate compared to the worldwide average equates to 94,059 additional UK deaths. That’s more the entire population of Stevenage, Darlington or Halifax wiped out. The UK government response, as well as the NHS’ medieval clinical response, are the reasons for this, with non-surgical face coverings being one of the two key factors.
After 18 months of following government ‘guidelines’ and everything that the government and NHS have done, the UK still has a COVID-19 mortality rate 3.27-times greater than the worldwide average. 94,059 individuals have died because of what the government told them to do, as well as what the NHS failed to do, as we set out in January and May this year. For this reason alone, the government and NHS have absolutely no credibility and no authority to tell a population what to do when those who do it are 3.27-times more likely to die.
As we explained earlier this month, viruses of the coronaviridae family have been in circulation and pathogenic to humans for approximately ten millenia, with the beta genus of SARS-CoV-2 being pathogenic for approximately 7,162 years. Throughout this period, technically so long that in periodization terms it is an epoch, until 2019 coronaviruses had managed to kill a total of 1,659 people. In more than 10,000 years.
So why have so many died since SARS-CoV-2 became pathogenic (remember that the base genome for SARS-CoV-2 can be traced back with high confidence to 1948 at the latest, potentially much nearer to 1900, it just was not pathogenic until recent years) when coronaviruses are seasonal irritants and nothing more?
The Virus:Host Interface.
Lifestyle and Western diet are the most important considerations but this is at the virus:host interface. In other words, an individual’s lifestle and diet contribute to dysfunction of the renin-angiotensin system; overexpression of inflammatory adipokines; leptin resistance; overexpression of linoleic acid (particularly in respect of its oxidisation to 4-hydroxy-2-nonenal and its role in the inhibition of dimethyarginine dimethylamine hydrolase, which regulates endothelial nitric oxide synthase); excess production of prostaglandin E2 and systemic collapse of a healthy n6:n3 ratio. This firstly presents the two greatest COVID-19 comorbidities that encourage disease progression and severity – hypertension and diet-induced obesity – and secondly prevents the immune system from mounting an effective innate response due to endemic level of vitamin D deficiency in the UK and other countries with similar deficiency, which we identified fourteen months ago. With SARS-CoV-2 having some effective means of evading detection by the innate immune system, this puts those with comorbidities at even greater risk. SARS-CoV-2 has shown in context the relevance of personal responsibility in that there are consequences of poor diet, lack of exercise and diet-induced obesity.
Discount the virus:host interaction and you can focus on how the government response antagonised a normally mild, seasonal respiratory virus, similar to the other common cold-causing coronaviruses HCoV-NL63; HCoV-229E; HCoV-OC43 and HCoV-HKU1.
Everything about SARS-CoV-2 revolves around the upper respiratory tract. In respect of its pathogenesis, it is all about avoiding high viral load in the upper respiratory tract in the early stage of infection. The two central components of the government response – lockdown and the enforced wearing of non-surgical face coverings – both cause an increase in viral load, to the point where an individual at the end of the crucial week one of the infection cycle, switches from moving toward viral clearance to moving toward COVID-19 disease progression. At that point, if they remain in a lockdown environment or continue to wear a non-surgical face covering, they exacerbate disease progression and increase their disease severity. In simple terms, they make themselves more ill.
In respect of the first factor, we have analysed and evaluated the negative health outcomes of lockdown on several occasions and the results can be read in previous articles from April 2020 through September 2020 and October 2020 to January 2021.
Background To Non-Surgical Face Coverings.
In respect of non-surgical face coverings, we first identified the serious risk they pose in September 2020, a little over one year ago. The original case for ‘masks’ was ambivalent at best, with the UK government’s own website stating that they “could” and “in certain circumstances” reduce the risk of infection or transmission. Note the use of the irrealis mood voice or conditional mood, the language of ‘could‘, ‘might’ and ‘up to’, the language used by Chris Witty in his poor attempts to lie and act like an expert who knows what they are talking about. As soon as you use the irrealis voice you are no longer talking fact and therefore are not talking science. Science is fact. Chris Witty talks sciency fiction, the speculative predictions of epidemiologists for whom the answer to any question, even before it is asked, is always the worse possible outcome where ‘up to everyone could die’. In contrast, when the realis voice or indicative mood is used, the language of ‘does’, ‘is’ and ‘will’ mean you are talking about fact and therefore about science.
Non-surgical face coverings by their name are neither surgical masks nor personal protective equipment. Even surgical masks or PPE conforming to N95/FFP2 only filter to 0.3 microns compared to the SARS-CoV-2 virion’s 0.12 micron size. So if PPE won’t stop virions on the way in, a piece of material made in China and strapped over the wearer’s face has no chance.
Picking a page one ranking search result for ‘face mask’ retailers, the product comes with an unsurprising description:
“Masks are not designed or intended to prevent, mitigate, treat, diagnose or cure any disease or health condition, including COVID-19/Coronavirus. They are non-sterile and are not intended for use in any clinical or surgical setting. Masks are not surgical masks, personal protective equipment, or filtering respirators (such as N95 masks).”
As we explained in June, SARS-CoV-2 is not airborne spread. Any respiratory particle large enough to carry sufficent virions to pose infection risk is a droplet and droplets are subject to both gravity in general and Stokes Law in particular. Any respiratory particle smaller than a droplet becomes aerosol residue upon exhalation and is too small to carry sufficient virions to pose an infection risk, either through direct inhalation or fomite transfer.
The issue is in exhalation.
Restricting The Effective Function Of The Respiratory System.
Depending upon your choice of taxon, i.e. how far up the taxonomic tree of human evolution you want to select as baseline, humans (homo habilis on) have existed for around 2 million years. Go back to simiiformes and you’re talking around 40 million years ago. The relevance here is that as just humans we have two million years of development and refinement of our respiratory system. At the risk of stating the obvious, we breathe air to survive though gas exchange and so our respiratory system is arguably one of the most, if not the most, important of our biological systems.
We can augment or artificially alter the function of the respiratory system, e.g. a diver or firefighter using a self-contained breathing apparatus or someone with low oxygen saturation being given a mask for oxygen assistance. However, none of these measures are designed to be used for a sustained period of time as they interfere with the normal, effective function of the respiratory system. As an observation, there is a high positive correlation in COVID-19 patients between the use of invasive, mechanical oxygen assistance, i.e. ventilators, and post-recovery pulmonary damage. McGroder et al. show a 3.6-fold increase in reduced lung function, ranging from decreased diffusion capacity, loss of muscle grip to chronic fibrosis. The UK government and NHS grandstanding over the challenge to get companies to manufacture ventilators was completely the wrong response. Oxygen concentrators were always – and remain – the more effective and far safer solution. Remember that the Chief Scentific Officer for the NHS effectively banned NHS hospitals on 2nd April 2020 from requesting urgently-needed oxygen concentrators – urgently needed to help save lives – instead providing them with a Helleresque set of rules to ‘permit’ requests for their usage by patients at home post-discharge.
Is it any wonder that the vast majority of COVID-19 deaths were in hospital where individuals were admitted with moderate disease severity only to suffer subsequent disease progression and death? Failure to default test upon hospitalisation with COVID-19 disease progression for PCT, CRP, IL-6 and aPL antibodies, as well as the NHS’ ignorant and arrogant refusal to accept the significant benefit of calcifediol in reducing mortality rate by over 50%, resulted in the deaths of tens of thousands.
The wearing of a piece of material over the mouth and nose means that sputum and mucal ejecta will be caught on the inside of the non-surgical face covering, as they are too large to travel through the material. Instead they will lie in the material, accumulating as the wearer breathes out, then to be re-inhaled as the wearer breathes in. In the event of any infection with SARS-CoV-2, the wearer is then unable to achieve viral clearance, the very thing that the respiratory system is trying to achieve. Strapping a piece of material over the mouth and nose limits the effective function of the respiratory system and restricts its capability to eject infected sputum and mucus.
Do you think your respiratory system functions better on an unrestricted basis or a restricted basis?
At this point one could posit that if non-surgical face coverings were effective then they would have reduced the mortality rate after their enforced imposition on the UK population as the government and NHS – along with just about every sign and notice affixed to every door, window and wall on every building – told people that face coverings would keep them safe and stop the spread of SARS-CoV-2. They did not, as the chart below shows:
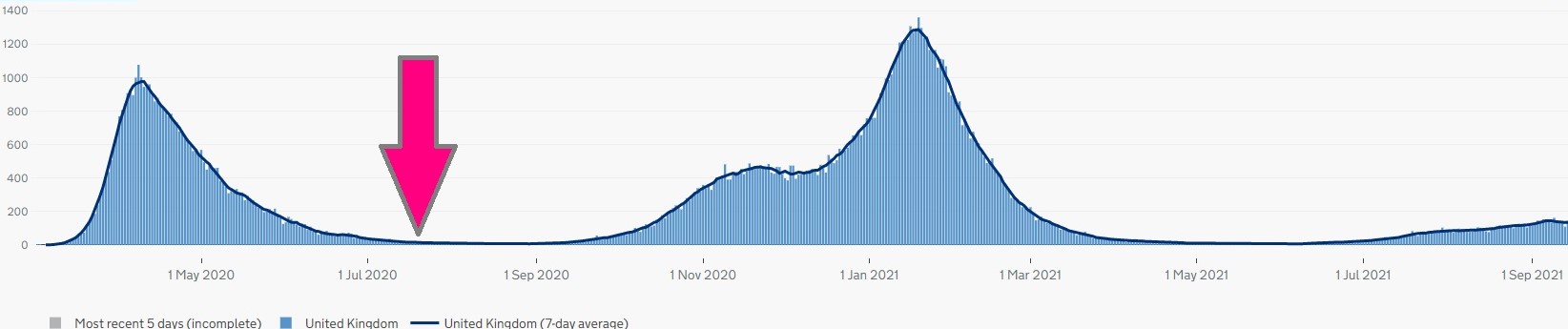
UK COVID-19 deaths with the point arrowed where enforced wearing of non-surgical face coverings became mandatory. Source: UK government and ONS.
The chart proves that non-surgical face coverings were ineffective and made little, if any, difference especially when you consider that SARS-CoV-2 is effectively inactivated in ambient temperatures above ∼20’c [Uddin et al., 2020], meaning it is inactivated in the summer and autumn as it is a seasonal irritant. This is unsurprising but subsequent research and studie shows that an additional risk was present – and remains so – in the form of microbial co-infection.
Viral And Bacterial Co-Infection.
Despite having several means of immunoevasion, as we set out here, SARS-CoV-2 is detected by pattern recognition receptors (PRRs) TLR7, TLR8 – and on a good day TLR3 – as well as NLRP3. It is therefore curious as to why those with low COVID-19 disease severity show only increased activity from these viral PRRs whereas those with high COVID-19 disease severity show additional activation of PRRs TLR4 and TLR9, which detect bacterial infection.
The co-existence of bacterial and viral PRRs indicates co-infection. This is separate to the increased expression of complement factors C3a and C5a following viral infection, as explained last month. The co-infection being bacterial is supported further by the increased creation of neutrophil extracellular traps (NETs) as part of the innate immune response, which are at greater levels than those one would expect to see in the response to viral infection.
This means that individuals with high COVID-19 disease severity also have bacterial infection. This infection initiates an innate immune response based upon the initial detection by the respective PRRs, meaning that both viral and bacterial-based innate responses are underway simultaneously. The effect of this is for the receptors wihtin each distinct response – the innate receptor activation pattern – to combine. In simple terms, this is like the ripples from two pebbles dropped into a lake coming together and creating an interference pattern. In respect of the innate immune system, this ‘interference pattern’ is multiple innate receptor activation patterns working at the same time and since they are pro-inflammatory in nature, increased cytokine signallng. This is particularly relevant around TLR4 as along with TLR7 and TLR8 it activates myeloid differentiation primary response protein 88, which stimulates interleukin 6 and tumor necrosis factor alpha. IL-6 and TNF-α are two of the main pro-inflammatory cytokines that when uncontrolled or hyperproduced cause cytokine storm. Cytokine storm can induce septic shock and is one of the main causes of COVID-19 mortality.
While the immune system is very efficient, it can be overwhelmed or inadvertantly initiate innate receptor activation patterns that individualy are effective in their own right but that when combined synergise. This synergy results in a ‘turbocharged’ overall response – the overproduction of cytokines leading to cytokine storm – or an out-of-balance response, where the ability to modulate the response – activate then inhibit the various stages – is compromised. The combination of innate receptor activation patterns triggers immunpathology which in turn increases COVID-19 disease severity, which would not otherwise, i.e. in the absence of bacterial infection, be the case.
Non-Surgical Face Coverings As Material Petri Dishes.
Unlike a virion a bacterium can survive without a host cell. However in order for the bacterium to multiply it requires specific factors. There are four generally accepted factors: temperature, moisture, oxygen and an environment with a tolerable acidity. The additional two are time and food.
Non-surgical face coverings present the ideal, if not perfect, environment for bacterial culture. A non-surgical face covering is not sterile to start with and therefore it becomes an increasingly dirty environment. As it is placed over the mouth and nose the ph level of the environment is ideal. It picks up moisture and temperature when placed over the nose and mouth, as well as a source of nutrients. It is exposed to oxygen constantly. And the longer it is worn or kept around the neck, in a bag or pocket, the more time there is for bacteria to multiply.
Wearing a non-surgical face covering provides all of the necessary conditions for a bacterial population to flourish. In turn, when the non-surgical face covering is worn for lengths of time, the bacteria will be inhaled as well as any newly-replicated SARS-CoV-2 virions re-inhaled because they cannot be exhaled normally. This is what causes the co-infection. In the same way as the longer someone wears a non-surgical face covering the higher any viral load, the longer someone wears a non-surgical face covering, the higher the bacterial incubation on the material.
Sustained wearing of a non-surgical face covering can cause bacterial infection. In the event of any SARS-CoV-2 viral infection, sustained wearing of a non-surgical face covering will increase the viral load. The combination of viral and bacterial infection triggers multiple innate receptor activation patterns, which leads to excessive cytokine production that leads to cytokine storm. While this will often be diagnosed as high COVID-19 disease severity, the activation of bacterial PRRs shows that the level of disease severity has been influenced by the wearing of a non-surgical face covering.
The sustained wearing of a non-surgical face covering is akin to putting a non-sterile dressing over a wound and leaving it there, taking it off and allowing it to lie around in a non-sterile environment before putting the same dressing back over the wound.
Conclusions.
- Non-surgical face coverings “can” “in some circumstances” reduce the risk of viral transmission.
- Non-surgical face coverings will increase viral load in the upper respiratory tract, to the level where the innate immune response is overwhelmed and the infection spreads to the lower respiratory tract. This causes COVID-19 disease progression that would not otherwise occur.
- Non-surgical face coverings will cause bacterial infection and in the event of SARS-CoV-2 or other RNA-based viral infection will cause COVID-19 disease progression and severity that would not otherwise occur.
- Wearing a non-surgical face covering makes the situation worse.
If you really want to wear a non-surgical face covering because it provides you with the confidence to go to the shops then that is your decision and should be respected. However do not wear it for any longer than is absolutely necessary and discard it after each use, replacing it with another. If not, you risk making yourself more ill in the event of any infection through the combination of innate receptor activation patterns.