We All Grew Up With Coronaviruses, As Did All Our Ancestors.
To understand the relevance of mortality rate, you have to appreciate that coronaviruses first became pathogenic to humans in the range 12,000 – 10,000 years ago, as a consequence of the first interaction between humans and livestock that occurred in the early Holocene. Mankind started to farm animals that are natural reservoirs for coronaviruses and over time there was zoonotic transfer. The alpha genus made the species jump around 10,000 years ago with the beta genus phylogenetically evolving approximately 2,850 years later.
The pathogenesis of these viruses – highly infectious but with very low infectivity – meant they became endemic and common, contributing to why they are called the ‘common cold’. Coronaviruses account for 15% – 20% of all common colds and around 30% of seasonal respiratory viruses. If you think of the general living conditions and environmental factors 7,150 – 10,000 years ago, not to mention the complete lack of any healthcare system; medical treatments and even awareness of the immune system, the fact that our ancestors didn’t die of these viruses should be an indicator of just how dangerous they are not.
Over the ensuing 7,150 or so years, nothing much changed and we have lived with four pathogenic coronaviruses; the two alpha genus – duvinacovirus HCoV-229E and setracovirus HCoV-NL63 – and the two beta genus; embecovirus (or lineage A beta) HCoV-OC43 and HCoV-HKU1.
Total Coronavirus Deaths Before 2019.
Based on the assumption that SARS-CoV-2 became pathogenic in 2019 (as opposed to was newly-discovered in 2019 having become pathogenic several years before, likely in 2013/14, as we first posited in September 2020), then over the previous 10,000 years, viruses of the coronaviridae family had killed a total of 1,659 individuals: these were from the SARS-CoV and MERS-CoV infection outbreaks in 2002 and 2012 respectively. Using WHO data, the combined number of individuals who were infected across both outbreaks is 12,329. This equates to a mortality rate of 13.5%, which reflects the pathogenesis and pathophysiology of both: low infectiousness and high infectivity. The inverse of SARS-CoV-2.
So, having managed to kill pretty much nobody for 10,000 years, a coronavirus decides to do nothing different – high infectiousness but low infectivity – but becomes the most dangerous virus ever in the history of the world (thankfully we are no longer forced to listen to the uncontrolled lies and incompetence of Matt Hancock). From an evolutionary biology perspective, this makes no sense. None whatsoever.
SARS-CoV is a sarbecovirus beta genus and MERS-CoV is a merbecovirus beta genus. While SARS-CoV-2 shares approximately 79% of its genome with SARS-CoV – although this figure varies hugely if you compare specific components of the genome, such as the receptor binding motif or receptor binding ridge loops – SARS-CoV-2 binds to apical ciliated epithelial cells in the upper respiratory tract and has a furin cleavage site, showing high affinity for transmembrane protease serine 2 (TMPRSS2). In contrast, SARS-CoV doesn’t and binds in the lower respiratory tract, plus MERS-CoV’s binding receptor is dipeptidyl peptidase 4 on non-ciliated bronchial epithelial cells. In simple terms, SARS-CoV and MERS-CoV were slow-moving, heavily-armoured viruses whereas SARS-CoV-2 is a fast-moving lightly-armoured virus. We first defined this difference in September 2020, over a year ago.
If you understand SARS-CoV-2 then you know it is a seasonal irritant and if you leave it alone, it has a single stage pathogenesis confined to the upper respiratory tract. If you do not understand it and/or try to fight it with lockdown, social distancing and non-surgical face coverings, you simply play into its hands by increasing viral load in the upper respiratory tract. This mediates a dual stage pathogenesis. Lockdown and enforced, sustained wearing of non-surgical face coverings increases viral load. It increases it to the degree where at the crucial pivot point at the end of week one of the infection cycle, an individual shifts from the innate immune response’s default position of moving to viral clearance to the government response-induced position of COVID-19 disease progression and severity.
The Government and NHS clinical response is what has caused the UK COVID-19 death toll, which should be in the range 20,000 – 25,000 (based on average seasonal/winter flu deaths and the worldwide average COVID-19 mortality rate), to exceed 134,000. Boris Johnson, Matt Hancock and Chris Witty are responsible for these deaths. Nothing short of genocide.
SARS-CoV-2 In Context.
The generally accepted mortality rate for winter or seasonal flu (influenza A(H1N1/H3N2)) is 0.5% – 2%. Throughout the 20th century, ignoring the sixth cholera pandemic that began in 1910, the three pandemics with the greatest loss of life have all been from influenza A. This of course ignores the accumulation of annual deaths worldwide from pathogens such as tuberculosis, cholera, dysentery and malaria: these deaths principally affect third world countries and undeveloped economies which may be why they are ignored. £37 billion wasted on a pointless, ineffective and unnecessary track and trace programme could have been used to effectively rid the world of many of these pathogens and save millions of lives but as they only affect Johnny Foreigner, the money instead gets awarded to the friends and associates of government ministers.
The worldwide mortality rate for COVID-19 (@0500UTC today, source: Johns Hopkins Coronavirus Resource Center/Worldmeters) is 0.0596%. Using the WHO range for influenza A mortality, the COVID-19 mortality rate is therefore in the range 8.4-times to 33.6-times lower. 0.0596% is also almost identical to the 0.05% percentage of the UK population (source: NHS) who have Type I hypersensitivity, more commonly known as immediate reaction hypersensitivity or anaphylaxia. We first offered this comparison in November 2020, as it puts into context the over-reaction and hysteria over SARS-CoV-2.
Type I hypersensitivity is the most serious anaphylaxia, as Th2 cells upregulate IgE isotype antibodies, which bind to mast cells and basophils, triggering the acute degranulation and release of histamine and serotonin neurotransmitters and excessive pro-inflammatory signalling. We know a lot about anaphylaxis and how it can be controlled in those with immediate reaction hypersensitivity, for example carrying an auto-injector pen, usually referred to as an EpiPen (short for epinephrine pen), to provide an immediate vasoconstrictive antagonist to the vasodilative histamine. No social distancing; lockdown; enforced wearing of non-surgical face covering; societal destruction; mental distress to millions; lost education to millions more; lost employment, income or business to still millions more for these people, yet the number of people at risk is about the same (the percentages equate to 40,715 for SARS-CoV-2 and 34,156 for immediate reaction hypersensitivity, so a nationwide difference of 6,559 people).
Viral Infection And Disease Progression Alter Mortality Rates.
Globally, the pathogenesis of SARS-CoV-2 has remained virtually unchanged for the past ten months and its infectivity, i.e. mortality rate, has weakened. As we highlighted in November 2020, Active Cases were 99% mild/1% serious or critical and Closed Cases were 95% recovered/5% deaths. Again as at 0500UTC today, these figures are now:
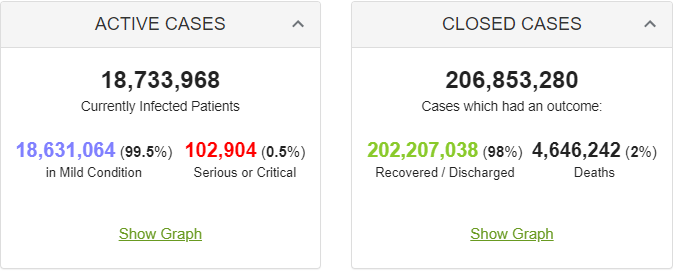
Source: Johns Hopkins Coronavirus Resource Center/Worldmeters.
Over the past ten months there have been numerous examples of phylogenetic evolution, with the emergence of Alpha, Beta, Delta, Eta, Iota, Gamma and Kappa. Politicians and healthcare professionals have been so quick to assert that these variants are more dangerous, which is incorrect unless you confuse infectiousness and infectivity. The above data provides an accurate, factual picture of what has been happening over the past ten months: SARS-CoV-2 has been attenuating, recombining in its constant attempt to maintain a fitness advantage – either through increased infectiousness or greater immunoevasion – as part of natural selection. It is evolving phylogenetically as it in effect reverts to its embecovirus/lineage A beta ancestry. It is regressing to become more like its common cold-causing relatives. The lowest common denominator to survive: the high infectiousness, low infectivity of the common cold.
Depsite everything that has been told to populations by increasingly desperate politicians, to try and justify their completely incorrect response in the first place (a response that is the case of the vast majority of COVID-19 deaths) over the past ten months, the COVID-19 mortality rate has fallen by 60%, as the Closed Cases Deaths has fallen from 5% to 2%. At the same time, COVID-19 disease progression and severity has fallen by 50%, as the Active Cases Serious or Critical has fallen from 1% to 0.5%.
The mass delivery of antivirals has no doubt helped contribute to these reductions, since the purpose of an antiviral is to attenuate symptomatic disease progression and severity. This ignores the harm done by antibody-dependent enhancement through type II hypersensitivity to polyethylene glycol PEG2000 in the lipid nanoparticle excipient and antiphospholipid syndrome from aPL autoantibodies binding to the phospholipid adjuvant in BNT126b2 and mRNA-1273 mRNA experimental vaccines. They are called experimental vaccines for good reason.
What is very stark in these figures though is that the percentage of populations at high risk of disease progression and severity is very low, with the mortality rate being even lower. As above, the COVID-19 mortality rate is 8.4-times to 33.6-times lower than that of influenza A. This should not be a surprise to anyone since SARS-CoV-2 has a burst size of 103 compared to influenza A that has a burst size of 6*103. This is virology101 yet appears to allude those supposedly in charge and even more supposedly knowing what they are talking about.
The Importance Of Paucisymptomatic Individuals.
As all of these figures are based upon COVID-19 disease progression, they do not include SARS-CoV-2 viral infection that does not lead to COVID-19 disease progression. This is as a result of the infection being overcome by the innate immune response within week one of the infection cycle. The exact number of individuals who catch SARS-CoV-2 and are asymptomatic is unknown but generally accepted to be around one third. Technically you cannot catch SARS-CoV-2 and be asymptomatic as multiple defences within the innate immune response are triggered: the signs of infection are there, e.g. increased cytokine signalling induced by TLR7, TLR8 and NLRP3, upregulation of complement factor C5a by P-selectin or increased creation of neutrophil extracellular traps, but they are just too tiny to be detected by the individual. The crumpled £5 note you found in your coat pocket was there all the time, you just didn’t feel it. It is the same for asymptomatic – or to give it its correct term, paucisymptomatic – individuals.
The COVID-19 mortality rate is calculated solely from a universe of individuals who have COVID-19 disease progression and severity. In other words, if 100 people develop the disease and seek medical attention and 1 dies, the mortality rate is 1%. However, if 2,000 people caught the virus but only 100 of those developed the disease and sought medical attention and 1 died, the mortality rate for the virus is 0.05%. No difference in the number of deaths but a huge difference in the mortality rate. The number of deaths is the same but the mortality rate is 20-times lower. This is something we first raised in April 2020, almost eighteen months ago.
Therefore, as you are only measuring those with COVID-19 when calculating the COVID-19 mortality rate, in order to assess the bigger picture you must include firstly those who are are paucisymptomatic and secondly those who are mildly symptomatic but do not feel the need to seek medical attention, either because they choose not to go anywhere near a hospital or because they put their symptoms down to a seasonal respiratory virus, whether a common cold or flu, and just carry on.
These are people who have had SARS-CoV-2 but either not developed detectable symptoms of COVID-19 or have not presented at hospital. Using just this group and applying the 3:1 ratio, you must increase the size of the universe by one third as the universe is currently based only upon the two-thirds who have detectable disease progression. This reduces the COVID-19 mortality rate to 0.0397%. This places the COVID-19 mortality rate in the range 12.6-times to 50.3-times lower than seasonal/winter flu and is before you factor in the second group, i.e. all those who thought they had a cold or flu and did nothing. This is of course an unknown figure and when you have a mortality rate that can be shown already to be as low as 0.0397%, you can argue that it is approaching a level of being insignificant.
If you postulated that 20 people thought they had a cold or flu for every one who presented with COVID-19 disease progression or severity (the Active Cases figure indicates 200 would be a fair figure but let’s use just 20 to be really conservative), then the COVID-19 mortality rate reduces still further to 0.00298%. It is now starting to resemble the 2009 influenza A(H1N1) pandemic. In August 2020, now over one year ago, we reflected on the similarities betwen this and SARS-CoV-2. The 2009 pandemic was the greatest single pathogenic event in human history with 10.2% – 20.4% of mankind being infected. Yet the total deaths was 18,449, giving a maximum mortality rate of 0.000027%.
Conclusions.
Certain groups of people are at increased risk of COVID-19 disease progression and severity arising from SARS-CoV-2 infection. These groups include those;
- with high viral load, as a result of being in close proximity to the same people for sustained periods of time, also known as lockdown.
- with high viral load, as a result of sustained re-inhalation of virions and restricted exhalation preventing viral clearance, from wearing non-surgical face coverings.
- with polymicrobial co-infection, as a result of multiple innate receptor activation patterns being triggered following bacterial cultivation on non-surgical face coverings.
- unable to adopt or maintain trained innate immunity, as a result of social distancing preventing persistent antigen exposure and causing a loss of effective function, especially cross-reactivity, within the innate immune response.
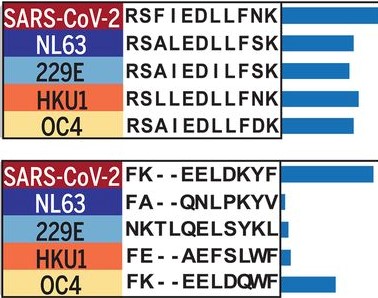
Cross-reactive epitopes of SARS-CoV-2 and the other four common-cold causing coronaviruses [Shrock et al, 2020].
- with vitamin D deficiency, as a result of following Public Health England guidance over the past decade and staying indoors to avoid the sun.
SARS-CoV-2 is a seasonal irritant, just like its common cold-causing coronaviridae family relatives. It poses considerably less danger to those at high risk of seasonal respiratory viruses than seasonal/winter flu. Unless you intefere with the innate immune system’s capability to response to it and/or allow viral load to accumulate to a high level in the early stage of viral infection.
Without the UK government and NHS response, COVID-19 has a mortality rate 12.6-times to 50.3-times lower than seasonal/winter flu. With the UK government and NHS response, COVID-19 has a mortality rate 3.29-times higher than the worldwide average.