SARS-CoV-2 Was Waving A White Flag By June 2020.
Since the onset of the Great Insanity we have been following the COVID-19 mortality rate and total deaths on a daily basis, as mortality rate is ultimately the best measure of infectivity, i.e. the damage to human health that a pathogen can cause. For an explanation of the difference between infectiousness and infectivity, read N501Y Is More Infectious But NOT More Dangerous from January 2021.
SARS-CoV-2 technically gave up some time between March and June 2020, when a single nucleotide polymorphism at position 23403 in its genetic sequence created the D614G amino acid substitution that allowed SARS-CoV-2-SG614 to become the dominant, fixed global variant in under three months, at a time when there was virtually no international travel, as we first identified in March 2021 and evaluated in greater detail in January this year within How Each Of Us Causes Every Variant. G614 saw the RBD undergo a significant change in its conformation from ‘3-down’ to ‘1-up‘ [Walls et al.; Weissman et al.; Yurkovetskiy et al., 2020]. While this increased infectiousness by a factor of 9-times compared to SARS-CoV-2-SD614 it a) did so without any increase in infectivity [Groves et al.; Korber et al.; Zhang et al., 2020] and b) post increased S1 subunit shedding, it increased presentation of exposed, unprotected RBD S2 subunit, making it easier to detect by and more vulnerable to attack from the immune system. We evaluated this in January 2021 in More Infectious Equals More Vulnerable.
At the same time, we now know that host-mediated editing by the apolipoprotein B mRNA editing enzyme, catalytic polypeptide-like (APOBEC) and adenosine deaminases acting on RNA (ADAR) families of enzymes was at work, causing the amino acid substitutions that both created the subsequent SARS-CoV-2 variants but also – crucially – ensured they had no increase in infectivity. It is likely that ADAR-editing mediated the former and APOBEC-editing the latter, giving each variant an increase in infectiousness but with equal or lower infectivity. Were it not for SARS-CoV-2’s high fidelity replication as a result of the exoribonuclease contained in nsp14-ExoN, it is arguable that the whole thing would have been over even sooner as nsp14-ExoN is a defense mechanism against nucleotide editing by the innate immune system as one of its anti-viral countermeasures. In effect this made each variant more transmissible and infectious but less likely to cause COVID-19 disease progression and severity, as the virus’ replication cycle was being disrupted, especially as APOBEC-mediated editing occurs post-replication.
Global COVID-19 Daily Deaths On A Par With Tuberculosis Daily Deaths Solely In India.
This is proven by the chart of worlwide COVID-19 daily deaths;
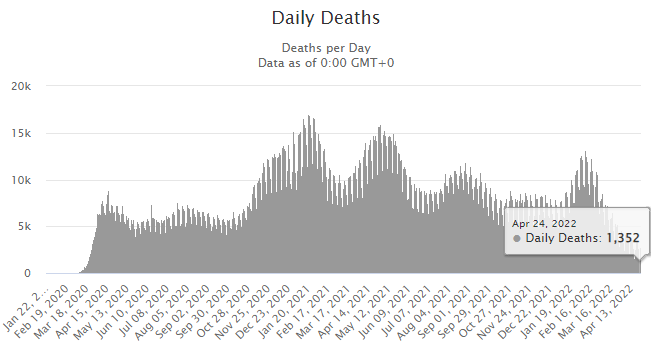
Source: Johns Hopkins Coronavirus Resource Center/Worldmeters.
which shows the daily deaths attributed to COVID-19 globally have been on a downward trend since late 2020 and are now as low as 1,352. To put this into context, it’s around the same level as the daily deaths from tuberculosis in India alone, based upon Ministry of Health and Family Welfare data that shows approximately 1,000 – 1,100 individuals die of tuberculosis in India every day. The WHO’s Global Tuberculosis Report 2021 calculates an even higher number, at approx. 449,700 deaths annually in India. Interestingly, India’s total COVID-19 deaths in the period March 2020 – April 2022 is 522,374 (source: Johns Hopkins Coronavirus Resource Center/Worldmeters), which equates to 250,739 deaths per annum. On this basis, tuberculosis kills 79.3% more people in India annually than COVID-19 has done or put another way, total COVID-19 deaths in India are 1.79-times lower than tuberculosis deaths.
At the current level, worldwide COVID-19 daily deaths are now 34.4-times lower than worldwide daily deaths from cardiovascular disease (source: HealthKnowledge). Even at their peak of 17,007 on 20th January 2021, COVID-19 daily deaths were 2.74-times lower than cardiovascular disease daily deaths. Tuberculosis is eminently treatable. Cardiovasular disease is preventable and in the majority of individuals is either treatable and/or the damage reversible. One has to ask the question why such endemic global diseases – tuberculosis and heart disease – are ignored in favour of COVID-19, which has a mortality rate in the range 4.1 – 16.6-times lower than influenza A [Wang et al.] and a worldwide mortality rate of 1 individual per 131,000 population, as we evaluated last month.
Active and Closed Cases.
In August 2020, COVID-19 Active Cases globally were 99% mild/1% serious or critical and Closed Cases were 95% recovered/discharged/ 5% died. By November 2020, Active Cases globally were 99.4% mild/0.6% serious or critical and Closed Cases were 97%/3%: within Closed Cases, there was a 40% reduction in the death rate over 3 months, as we set out in The Common Cold And SARS-CoV-2 Immunity. In January 2021 both Active Cases and Closed Cases remained unchanged however by September 2021, Active Cases were 99.5%/0.5% – a 16% reduction in serious/critical cases – and Closed Cases were 98%/2% – a 50% reduction in the death rate – as we set out in How Low Is The SARS-CoV-2 Mortality Rate?. Remember that from January to September 2021 we had seen the emergence of the second dominant, fixed global variant T478K, the lead amino acid substitution in B1.617.2/Delta variant, as we had predicted in July 2021, as well as the initial formation of the Omicron variant.
This is the current data for Active Cases and Closed Cases:
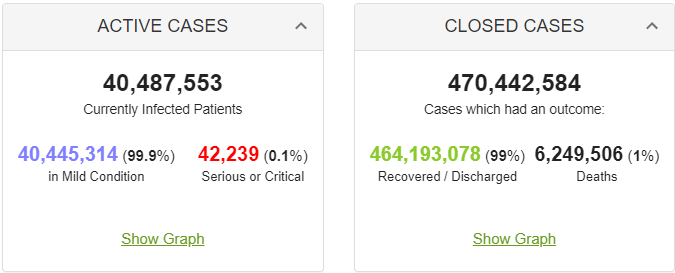
Source: Johns Hopkins Coronavirus Resource Center/Worldmeters, @0500UTC 29/04/22.
Active Cases are now 99.9%/0.1%, which is a 90% reduction since August 2020, i.e. through Alpha, Beta, Delta, Kappa and Omicron variants and all their increased infectiousness, infectivity has reduced by 90% and that’s from an already low baseline of 1%. Closed Cases are 99%/1%, which is a 80% reduction since August 2020, confirming the continuation of the trend reduction in daily deaths. This can be illustrated by overlaying the 7-day moving average onto the earlier chart;
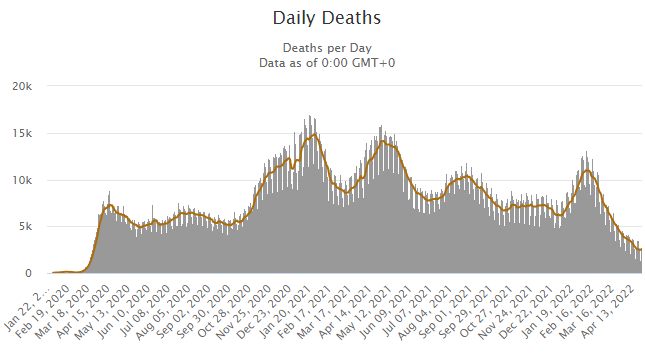
Source: Johns Hopkins Coronavirus Resource Center/Worldmeters.
Focusing on infectivity and the resultant deaths shows SARS-CoV-2 in its correct, true context. A seasonal irritant and nothing more. It poses a risk to specific groups, those with dysfunction in their renin-angiotensin system as a result of hypertension and diet-induced obesity, which we first identified and highlighted in October 2020 and expanded upon in July 2021 within COVID-19: The Western Diet Disease.
At anything other than high viral load in the early stage of infection that, in the event of viral infection, is mediated by being in close proximity to the same people for sustained periods of time, also known as lockdown [Kidd et al.; Volz et al., 2020] and/or sustained wearing of non-surgical face coverings, something we analysed in September 2021, SARS-CoV-2 is a seasonal irritant. From when we first identified its phylogenetic evolution in September 2020, SARS-CoV-2 has been regressing toward its embecovirus beta genus relative HCoV-OC43.
Even at their peak, COVID-19 daily deaths were still 2.74-times lower than daily deaths globally from heart disease and are now 34.4-times lower. Context is everything.